Back to: Trial Questions
Question:
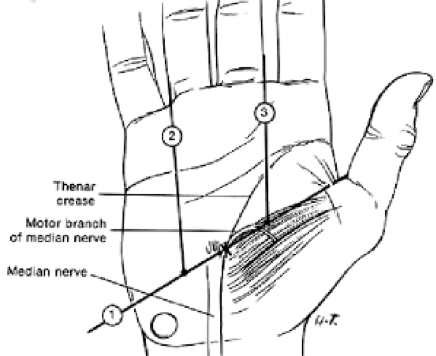
Describe this picture and what condition it is associated with
CTS Most common compressive neuropathy – median nerve underneath the transverse carpal ligament 9 tendons and 1 nerve Palmar cutaneous branch comes off 5cm proximal to wrist crease Recurrent motor branch has variable anatomy to supply LOAF muscles (see below) Kaplans Line Ulnar border of thumb 1 and 2nd web space Multiple causes idiopathic / physiological / mass effect / systemic illness / inflammatory Typical symptoms – nocturnal pins and needles, dropping things Signs – look – wasting thenar muscles – feel – sensation decreased tips of thumb and index – move – test (ABPB) – sp. tests – Tinels / Phalens / Durkins Diff Pronator Syndrome – also look forearm muscles wasting / sensation palm of hand / pain on resisted pronation C6 radicuopathy – test wrist extension / sensation lateral border forearm CMCJ OA – tenderness over base of thumb / +ve grind test Confirm with NCS (if doubt) Motor – prodromically / stimulus electrode placed proximal to CT and recording electrode placed on AbPB muscle (+ indifference and ground electrodes on other fingers) Positive if – increased latency >4ms / decreased amplitude <5mv Management Non operative – info sheet / night splint Diagnostic injection 2mls 0.5% marcaine and 40 mgs depomed (2cm proximal wrist crease and ulnar to PL tendon) – use if clinically a bit equivocal and NCS normal (does happen) Operative (see above) Open release gold standard – 90% success Grip strength 3/12 to return Beware scar tenderness / pain J Hand Surg [Am]. 1998 Sep;23(5):852-8
Describe how you would do a carpal tunnel release
Marked and consented Patient supine / arm table – local anaesthetic 10mls 1% lignocaine infiltrated with blue needle – field block High arm tourniquet but more pleasant for the patient if one is not used – explain to patient Loope magnification Prep and drape Check the local anaesthetic Longitudinal incision in line with radial border of ring finger just ulna to prominent crease – no further distally than Kaplan’s cardinal line Down through skin and subcutaneous tissue 3 by 4 pronged self retaining retractor in – key to operation is to keep tension on tissues Cut with sharp dissection through the transverse carpal ligament When the carpal tunnel is reached use a MacDonald underneath to protect the median nerve and open it up Use scissors distally Use MacDonald and blade proximally to complete release Check median nerve is free Close with 4,0 vicryl rapide interrupted sutures, mepofix dressing and crepe bandage ElevateAnswer:
Please discuss the anatomy of the recurrent branch of the median nerve
The anatomy of the recurrent branch of the median nerve. 101 cadavers disected to spatially define the origin and course of the recurrent branch of the median nerve The recurrent branch of the median nerve was classified into 3 types. Type I passed through the TCL; it is rare, occurring in 7% of the specimens. Type II nerves (74%) passed distal to the TCL through separate obliquely oriented fascia that originated on the TCL and inserted on the undersurface of the palmar aponeurosis. Type 111 (19%) passed distal to the TCL, but did not pass through the obliquely oriented fascia. 99% originated either from the central portion of the median nerve or just radial to it. There were no ulnar origins. 4% had more than 1 recurrent branch. The variability in the literature on the anatomy of the recurrent branch can be accounted for by failure to properly identify the TCL as being separate from the obliquely oriented fascia distal to the TCL through which the nerve frequently penetrates. This study concludes that the transligamentous branch (type I) is uncommon and the reported high incidence of branches passing through the TCL can be explained by mistakenly combining recurrent nerve types I and II.